Aldosterone (C21H28O5) is a compound of hormone mineralocorticoid hormone secreted by the cortex of the gland adrenal gland. It is part of the renin angiotensin aldosterone system or RAAS and is an integral part of the complex mechanisms that control water and electrolyte balance within the body. Its action affects the levels of sodium, potassium and water through the excretory and circulatory systems.
Function of aldosterone
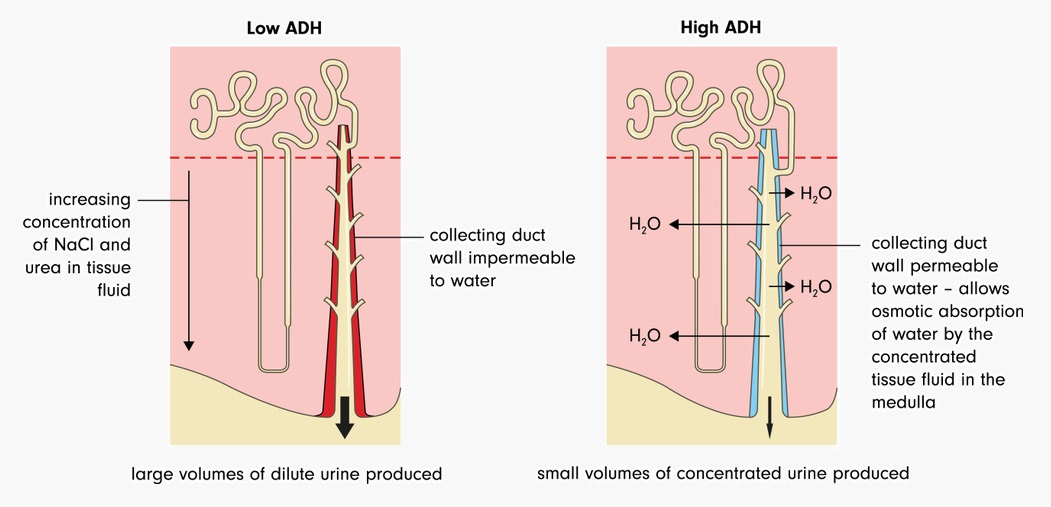
The primary function of aldosterone is to increase reabsorption within the last portion of the distal tubule of the nephron and collecting ducts. When working specifically at this location, the hormone binds to mineralocorticoid receptors on the distal tubule membrane. Once bound, it increases the permeability of the distal tubule membrane. This facilitates the passage of potassium and sodium. Aldosterone also activates the mechanism of secretion of hydrogen ions in the collecting ducts. This regulates plasma pH and is therefore important in acid-base balance. It is also understood that aldosterone plays an additional role in the release of antidiuretic hormone (vasopressin or ADH) from the pituitary glandso more water is reabsorbed into the body via the nephron. However, the aldosterone only affects about 3% of total water reabsorption. Therefore, it is considered a more appropriate adjustment mechanism for small, regular changes in blood volumes than a sparing measure of acute water loss. blood.
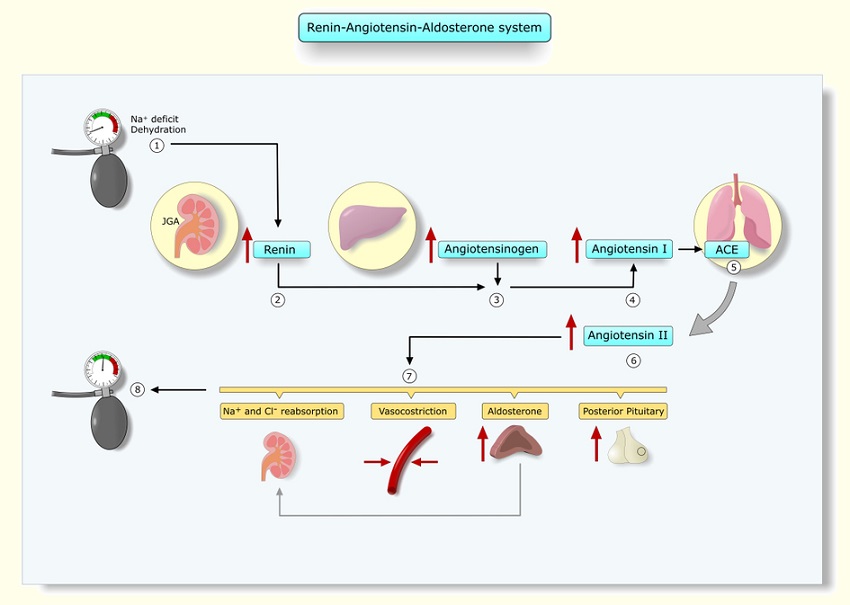
Aldosterone in the RAAS
The renin-angiotensin-aldosterone system or RAAS regulates blood pressure through a single pathway composed of several hormones. These hormones (renin, angiotensin and aldosterone) work together to produce the enzymes responsible for vasoconstriction and regulate the secretion and regulation of aldosterone. excretion in the kidneys. The RAAS works together with the RAS or renin-angiotensin system to rapidly control blood pressure when needed.
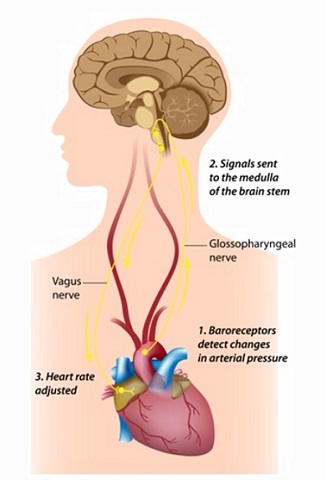
Renin or angiotensinogenase is an enzyme and a hormone produced by the kidney and is released when fluid levels in the body fall.. Hypovolaemia can be caused by dehydration, low water intake, prolonged diarrhoea or vomiting, blood loss and systemic infections. The kidney requires a signal to release renin. This is administered through the nervous system autonomic which responds to signals sent from specialised baroreceptor cells in the walls of the heart and main arteries. There are two types of baroreceptors: high and low pressure. They detect levels of stretch in arteries, veins or myocardium. The former is located in the aortic arch and carotid artery. The latter in the pulmonary arteries, larger veins and myocardium. When baroreceptors sense a drop in blood volume, renin is released. Renin converts angiotensinogen into angiotensin I.
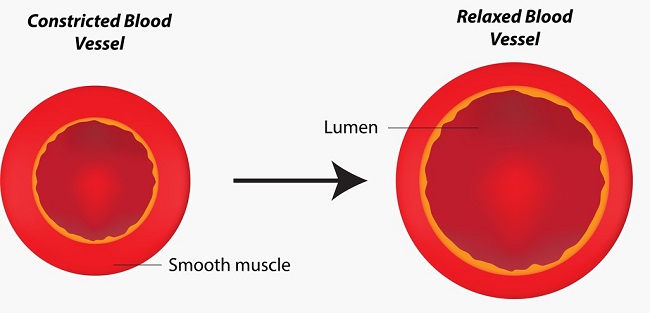
Angiotensinogen is a precursor protein and is manufactured in the liver. In the presence of renin, angiotensinogen is converted to angiotensin I, yet another precursor. To produce the final form, or angiotensin II, another enzyme produced by the lungs called angiotensin-converting enzyme, or ACE, is needed. The term ACE may sound familiar, as ACE inhibitors are popular drugs used to control chronic high blood pressure. By inhibiting this enzyme, blood vessels relax (see image below) and blood pressure does not reach dangerous levels. An ACE is released, angiotensin I is converted to angiotensin II.
Angiotensin II directly affects the walls of blood vessels, constricting them and raising blood pressure. It also ensures that blood is available to major organs such as the heart, kidneys and lungs. In the kidney, angiotensin II causes the arterioles that supply blood to each nephron to constrict. The afferent or supply arteriole contracts a little; the efferent or outflow arteriole contracts much more. This causes the blood between these vessels to flow backwards, a vital mechanism, since without continuous pressure, the exchange of ions, water and other molecules cannot take place within the nephron..
In addition to its effect on blood vessel musculature, angiotensin also increases the rate of sodium reabsorption within the nephron. Higher concentrations of sodium attract higher concentrations of water.. As more sodium is reabsorbed into the blood, the nephrons automatically reabsorb more water, increasing blood volume.
Angiotensin II also signals the release of aldosterone from the adrenal cortex. Aldosterone increases the volume of water that is reabsorbed back into the blood. circulatory system by allowing even greater reabsorption of sodium. In addition, both aldosterone and angiotensin II signal the release of antidiuretic hormone (ADH or vasopressin) from the posterior pituitary gland. As one of its names suggests, ADH is a vasopressor or vasoconstrictor. It also increases water reabsorption in the nephron as shown below.
Aldosterone versus ADH
While both aldosterone and antidiuretic hormone are hormones secreted to increase water volume within the body and both act in the distal convoluted tubules and collecting tubules of the nephron, this is where their similarities end.
ADH is a lipophobic and fast-acting peptide hormone. Aldosterone is a slightly slower acting (but longer acting) lipophilic steroid hormone, more specifically a corticosteroid hormone.
Aldosterone is synthesised and released from the adrenal glands; the prohormonal form of ADH is produced in the hypothalamus but released from the pituitary gland. Aldosterone also affects the movement of sodium molecules across the membrane of the nephron tubules by increasing their permeability, whereas ADH makes these membranes more permeable to water. This means that aldosterone increases the osmotic pressure and ADH allows water molecules to respond to this change.
The Baroreflex
When blood pressure levels rise, high blood pressure receptors send signals to the brain which reduce heart rate and dilate blood vessels. When hypovolaemia or sudden shunts of fluid from the circulatory system occur, as in syncopal episodes, low-pressure receptors in the pulmonary arteries, large veins, and atrial and ventricular walls do the opposite. They send signals to the brain that result in an elevated heart rate and vasoconstriction. Both reactions are known as baroreflexes. Depending on the location of the baroreceptors, the signals travel along the nerves and end up in the medulla oblongata.
To reduce blood pressure, the medulla oblongata activates the baroreceptors. parasympathetic nerves to reduce cardiac output. This occurs through a slower heart rate and contractions of the muscle cardiac muscle. At the same time, the medulla oblongata sends inhibitory signals to the sympathetic nerves which relax the walls of blood vessels and provoke vasodilation. This dilation means a larger space for the same amount of blood, leading to a reduction in blood pressure.
To increase blood pressure, the medulla activates sympathetic nerves that increase heart rate and the strength of myocardial contractions, which increases cardiac output. Parasympathetic nerves are inhibited through which the relaxing effect on the blood vessel walls is eliminated and the vessels contract. This pushes more blood production into a smaller space within the circulatory system and increases the pressure within the blood vessels.
The role of adrenoceptors in raising and lowering blood pressure
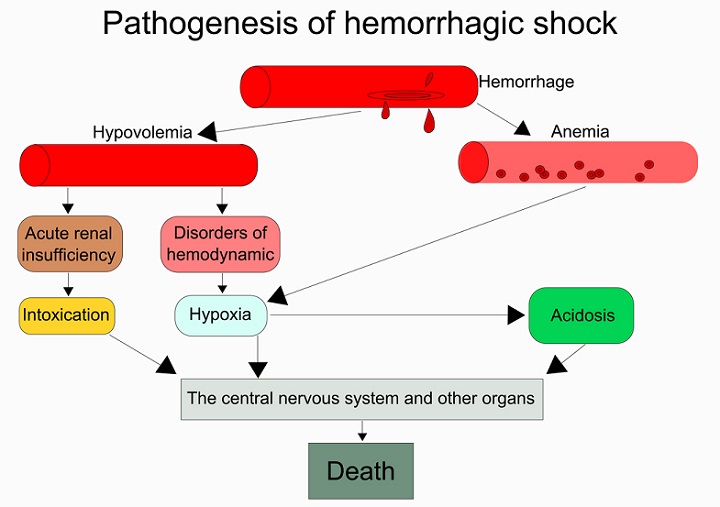
Other mechanisms are also involved when baroreceptors signal hypovolaemia. These have a greater effect than the RAAS and come into effect when pressures fall or rise well beyond normal ranges. The steps leading to haemorrhagic shock in cases of significant blood loss, for example, are shown below. Note how low blood volumes lead to renal failure due to the inability to maintain the pressure in the glomerulus and thus end any filtration.
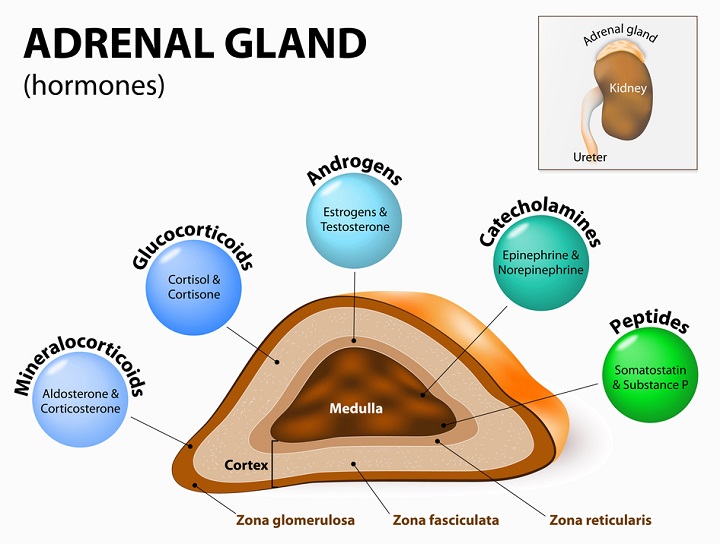
Adrenaline is released from a different region of the adrenal glands (the medulla), along with the neurotransmitter noradrenaline. These create alpha and beta effects to raise blood pressure. Alpha and beta adrenoreceptors are made up of two groups: 1 and 2. Alpha-1 adrenoreceptor agonists bind to alpha-1 receptors on peripheral blood vessels and cause their muscles to contract, diverting blood to more critical organs and systems. A agonist is a product which, when it comes into contact with an receiverinitiates a chemical response. Alpha-2-adrenergic receptor agonists bind to alpha-2 receptors and inhibit the release of norepinephrine (noradrenaline).
Thus, it has the opposite effect to alpha-1 function. Beta-1-adrenergic receptor agonists affect the myocardium, creating extra tachycardia and contractility, but also act to release renin, initiating the RAAS cycle. Beta-2-adrenergic receptors dilate blood vessels in critical organs and airways to increase oxygenation. Beta-2 pathways also increase glucose production and allow skeletal muscles to contract much more forcefully.
Aldosterone production
The adrenal glands are located above the kidneys and are also called the suprarenal glands. They produce a wide variety of endocrine hormones that act as chemical messengers within the confines of the body. Aldosterone is produced in the zona glomerulosa of the adrenal cortex just below the surface. The production of aldosterone requires an enzyme called aldosterone synthase.. Congenital deficiencies in aldosterone synthase and any other enzyme required for aldosterone production lead to hyponatraemia and hyperkalaemia. This shows that aldosterone primarily maintains the correct levels of sodium and potassium within the body.
Another ingredient of aldosterone is cholesterol. It is important that hormones are lipid-based so that they can easily and quickly enter the phospholipid membranes of the receiving cells. The interaction of cholesterol with a variety of enzymes can produce numerous steroid hormones. Steroid hormones or corticosteroids are classified into mineralocorticoids (aldosterone), glucocorticoids (cortisol) and sex corticoids (oestrogen, progesterone and androgen) according to their function. The image clearly shows the range of chemicals produced by the adrenal gland and where. At the top right, a small box shows the position of the adrenal gland above the kidney.
What is a mineralocorticoid?
Aldosterone is a mineralocorticoid, meaning that its action is involved in the maintenance of mineral levels. When activated, aldosterone binds to specific mineralocorticoid response elements (MREs) where they can increase the reabsorption of ions and water back into the body and prevent the excretory system. This translates into an increase in extracellular fluids, higher blood pressure and lower potassium levels in the body. As aldosterone is only responsible for small amounts of water, its contribution to extremely high or low blood pressure in the short term is minimal, but its consistent long-term action on water and mineral salt balance is crucial. This pivotal role can be seen in the symptoms of people suffering from adrenal disease.
Hyperaldosteronism
Overproduction of aldosterone by the adrenal gland is classified as primary or secondary. Primary hyperaldosteronism in both adrenal glands is due to an overproduction of aldosterone by the adrenal gland. hyperplasia bilateral adrenal hyperplasia or Conn’s syndrome (an adrenal tumour) and is rare. Unilateral primary adrenal hyperplasia is even rarer, as is the familial hereditary form.
Secondary hyperaldosteronism is more common than the primary form, but does not yet affect a significant percentage of the population. population worldwide. It is caused by hyperactivity in the RAAS system often resulting from oedema, renin-producing tumours, ascites and renal artery stenosis leading to low blood perfusion to the kidney even in the presence of normal blood volumes.
Symptoms of primary hyperaldosteronism (or primary aldosteronism) are few, but may progress to hypertension, hypokalaemia and hypomagnesaemia. Secondary symptoms of hyperaldosteronism then spread similarly from asymptomatic to high blood pressure and lower potassium levels. The more generalised symptoms that are often mistaken for other diseases are fatigue, pain in the arms and legs, and aches and pains. headachepolyuria, polydipsia and metabolic alkalosis. The aldosterone/renin ratio (ARR) blood plasma test is used to differentiate primary from secondary hyperaldosteronism.
Hypokalaemia is the result of increased sodium reabsorption in the nephron, an effect caused by the hormone aldosterone, and in doing so increases the volume of water within the body. As sodium is reabsorbed, potassium is excreted. Levels of magnesium can be low because the balance of electrolytes within the body is often co-dependent . Low levels of potassium are often accompanied by low levels of calcium and magnesium.
Hypoaldosteronism
Hypoaldosteronism is an equally rare disease that occurs due to aldosterone deficiency. This deficiency is classified as either hyporeninaemic or hyperreninaemic hypoaldosteronism, the accompanying levels of renin in the blood. The small number of people with this disease are usually renal, diabetic or severely ill patients. Other risk factors include intoxication by lead poisoning and heart medicines.
Long-term hyperkalaemia, a result of hypoaldosteronism, has a direct effect on the muscles, since the potassium is needed for muscle contraction. Symptoms of low aldosterone levels therefore include palpitations, muscle weakness and irregular heartbeat. Others are nausea and difficult to control fluctuations in blood pressure.
Blood pressure medications
Medications for hypertension are classified into different classes. The general functioning of the following classes has been discussed at some point in this article, as blood pressure medications work in one or more of the same regions as the RAAS.
ACE inhibitors
Angiotensin-converting enzyme inhibitors suppress levels of angiotensin, a major component of the RAAS. Lower levels of angiotensin mean less vasoconstriction. . ACE inhibitors are teratogenic; this means that the foetus of a pregnant woman taking this medicine will also experience low blood pressure, as well as hyperkalaemia and renal failure.
Beta-blockers
By reducing cardiac output, blood pressure is reduced. Beta-blockers reduce the rate at which the heart beats and the force of myocardial contraction. Beta-blockers are known to cause extremely slow heartbeats (bradycardia) of around 30 beats per minute and patients should be carefully monitored.
Angiotensin II receptor blockers.
Angiotensin II receptor blockers (ARBs) also act on the RAAS in much the same way as the ACE inhibitor group. The difference between an ACE inhibitor and an ARB is that the former limits the main ingredient of angiotensin II production that stops the conversion of angiotensin I to II, while the latter prevents the end product from binding to receptors in blood vessels. The effect of these two groups is essentially the same. However, the longevity of ACE inhibitors and the reluctance of pharmaceutical companies to replace them are leading to much debate about which of the two is the better option.
Diuretics
When blood pressure is high due to hypervolemia, usually due to obesity, stress, electrolyte imbalances, low levels of physical activity, chronic alcohol consumption, heart disease and kidney problems, diuretics can be used to lower blood pressure. diuretics can eliminate excess fluids through the excretion of sodium.. To do this and to avoid specific side effects, certain groups work at different levels. This is shown in the picture below, which shows the actions of the three main groups in different parts of the nephron.
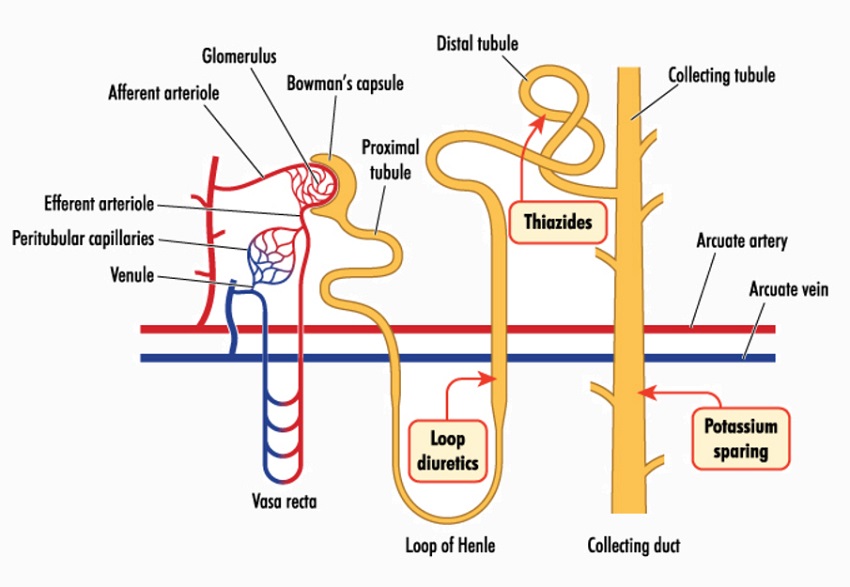
The three main groups are thiazide diuretics, potassium-sparing diuretics and loop diuretics. Thiazide diuretics inhibit the reabsorption of sodium and chloride ions early in the nephron (in the proximal segment of the distal convoluted tubule) but later, and partly due to the influence of aldosterone on the ion cotransporter proteins that allow the passage of salts across the tubular membrane, this effect is somewhat compensated. This compensation is not sufficient to override the sodium-lowering effect of the proximal segment, but leads to low potassium levels.
Potassium-sparing diuretics, the second group, were developed in response to the hypokalaemia experienced in patients prescribed thiazide diuretics. These drugs primarily affect the sodium-chloride balance. More sodium (and more water) is sent to the ultrafiltrate and potassium remains. Therefore, these drugs have the potential to cause hyperkalaemia.
The final group is composed of loop diuretics. They act very early along the nephron, at the end of the loop of Henlé (hence the name) and before the proximal convoluted tubule. This type of diuretic binds to cotransporter proteins to slow or stop the reabsorption of sodium and chloride ions. This is extremely similar to the mechanism of thiazides, but the early onset of effects along the tubule means that loop diuretics are much more potent. Consequently, thiazides are used to control high blood pressure in people with relatively good renal function; loop diuretics have a better effect in patients with low renal function and low filtration rates.
Vasodilators
With a central or local effect, through the vasomotor centre of the medulla oblongata or directly on the smooth muscle of blood vessels, vasodilators increase the size of the blood vessel lumen, creating a larger space in which blood can circulate and lowering blood pressure. Vasodilators are not a primary therapy for hypertension, but are used in combination with other drugs to lower blood pressure. As they also increase the blood supply to the heart, vasodilators are mainly used for cardiac patients.
Combined alpha- and beta-blockers
Dual alpha- and beta-receptor blockers or alpha-beta adrenergic blockers have a dual function. As alpha blockers, they relax the smooth muscle of blood vessels. As beta-blockers, they slow the heart rate and decrease the force of myocardial contraction. This dual mechanism can lead to dizziness when standing upright. standing abruptly or syncope when blood pressure is too low.