Atrophy is a term that describes the wear and tear of the tissue cellular. On a larger scale, you can see a reduction in the size and function of a muscle or a limb. This process is usually gradual and chronic, if not permanent. However, atrophy is not an exclusively pathological state. Atrophy is actually part of our natural homeostatic development. The wrinkles that appear on our face as we age atrophy, as does our thinning hair and the loss of teeth. There are many reasons why tissue can atrophy. It can be caused by age or geneticssuch as inheriting a defective set of genes that signal cell lysis or inhibit the assembly of a crucial protein. Another factor is environmental change. Depending on our health or income status, we may experience nutritional deficits. Or a physical injury may puncture our tissues or damage the nerves that innervate our muscles. Likewise, chronic diseases can permanently affect our tissues.
The inevitable consequence of tissue atrophy is that the ability of the affected limb to perform its functions is diminished. However, the actual degree of damage depends on its partial or complete effect and the subject of the atrophy. Atrophy that targets nerves or an extended muscle will affect the body systemically. This type of effect would result in pronounced deficits (i.e. multiple sclerosis). In fact, those suffering from atrophy often show two clinical signs: shortened limbs and body weakness.
Types of atrophy
While atrophy can describe a wide range of conditions, it can arise naturally or from disease. In fact, some presentations can occur for any reason. For example, the disuse atrophy is a progressive withering away of bones and muscles resulting from prolonged inactivity. In the event that a patient develops a chronic disease such as cancer or HIV, bone density and muscle mass are significantly reduced. Cachexia is a clinical name for an unintentional muscle loss that follows an illness or precedes death. Hence its colloquial name, “loss of muscle mass”. The same applies to bedridden patients with spinal injuries, paraplegia or sudden disabilities. However,Disuse atrophy can also occur in healthy individuals. For example, a student athlete may experience some disuse atrophy in the off-season of the sport he or she plays in the face of a reduced workload.
Symptoms of muscle atrophy?
- Generalised or localised weakness
- Numbness of the extremities
- Ataxia
- Pain
- Muscle spasms
- Unintentional weight loss
Pathological atrophy occurs in many areas of the body for a variety of reasons. We will delve more deeply into the common presentations, but it is worth mentioning that not all atrophy affects muscle. Atrophy can target connective tissue fibres such as tendons, bones, ligaments and fatty tissue. Neural diseases (such as multiple sclerosis or Parkinson’s disease) atrophy brain tissue and neural cells, or break internal connections. Glandular atrophy can occur with prolonged hormone or steroid excess or nutritional imbalance. So, it is quite involved and relies on an interplay of signalling events that are still being understood.
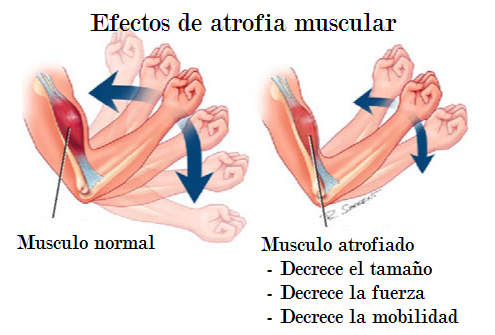
Muscle atrophy
Muscle atrophy typically refers to the weakening of the muscles skeletal muscles. These are the muscles that form the framework that move our limbs. They are also called striated muscles that perform voluntary movements. There are generally two types of muscle atrophy: disuse and neurogenic atrophy. Disuse atrophy is the result of muscle inactivity, as discussed above. When a weak, bedridden or paralysed patient does not use muscles enough, the inactive muscles will weaken from lack of use. This results in a gradual decrease in total muscle mass. However, disuse atrophy can also benefit from physiotherapy. In some cases, exercising the affected muscles can reverse the atrophy completely and better nutrition can aid the body’s recovery.
Neurogenic atrophy, on the other hand, is a more severe type. Unlike disuse atrophy, neurogenic atrophy will affect the muscles that are affected. nerves connected to the muscles rather than the muscles themselves. Nerve damage is much more difficult to treat and will not be reversed by exercise. Common causes of nerve damage include alcohol abuse, toxins and injury. Other examples of diseases that affect nerves involving muscle movement include ALS, polio, carpal tunnel syndrome and spinal cord injury. Diagnosis of muscle atrophy usually occurs in a physician’s clinic and includes measuring the size of the muscle in the affected limb and performing tests for blood testsMRI and nerve studies.
Muscle atrophy in the spine
Spinal muscular atrophy, or SMA, is an autosomal recessive spinal disorder that is carried by 1 in 40 people. CMA specifically atrophies the motor neuron cells of the spinal cord. Our spinal cord is rich in nerve cells that help coordinate our body’s movement. In fact, most of the neurons that control our muscles are found within our spinal cord. But, of course, atrophy eventually affects the muscles, as they gradually shrink in response to not receiving signals from the damaged nerves and are therefore inactive.
Since no two patients with CMA share exactly the same experience with the progression of their disease, CMA is classified into four categories.
Types of CMA:
- Type Ithe most common and severe type of CMA that is usually diagnosed before an infant is 6 months old.
- Type IIis diagnosed between 6 months and 2 years of age. It is often first noticed if a baby shows a motor delay or fails to achieve these milestones (i.e. the baby can sit up unaided, but will need help to sit up again. The baby will not be able to walk and will need a wheelchair).
- Type IIIalso called juvenile CMA, is diagnosed between 18 months and 3 years of age, or even in adolescence. Patients will progressively lose mobility until they need a wheelchair.
- Type IVis a very rare type that appears in adulthood. It is therefore said to have an adult onset that will result in mild motor problems. The age of onset is usually between 18 and 35 years.
Vaginal atrophy
Vaginal atrophy is a disorder that attacks the muscular lining of the vagina and urinary tract. Common symptoms include vaginal pain and painful intercourse. Low levels of oestrogen are to blame for vaginal atrophy. Oestrogen loss occurs during peri- or post-menopause, but also during lactation in new mothers. One artificial way in which oestrogen levels can be lowered is with long-term medications that treat oestrogen conditions such as endometriosis. Although the taboo surrounding vaginal conditions prevents many women from treating their symptoms, vaginal atrophy can be improved with vaginally administered oestrogen creams and lubricants.
